Every aspect of the immune system plays a unique and integral role in protecting the body against germs and infections. Our immune system is a collection of cells, tissues, and organs. As these functions work together, they not only combat disease but also ensure the overall well-being of your health. The body is an adequate environment for pathogens like viruses, bacteria, parasites, and fungi are survive. The immune system fights towards eliminating access to such microbes and prevents them from growing and causing health issues.
While a majority of people understand the primary function of an immune system, there remain many facts that they might not be aware of yet. These are the most interesting and lesser-known facts about the immune system.
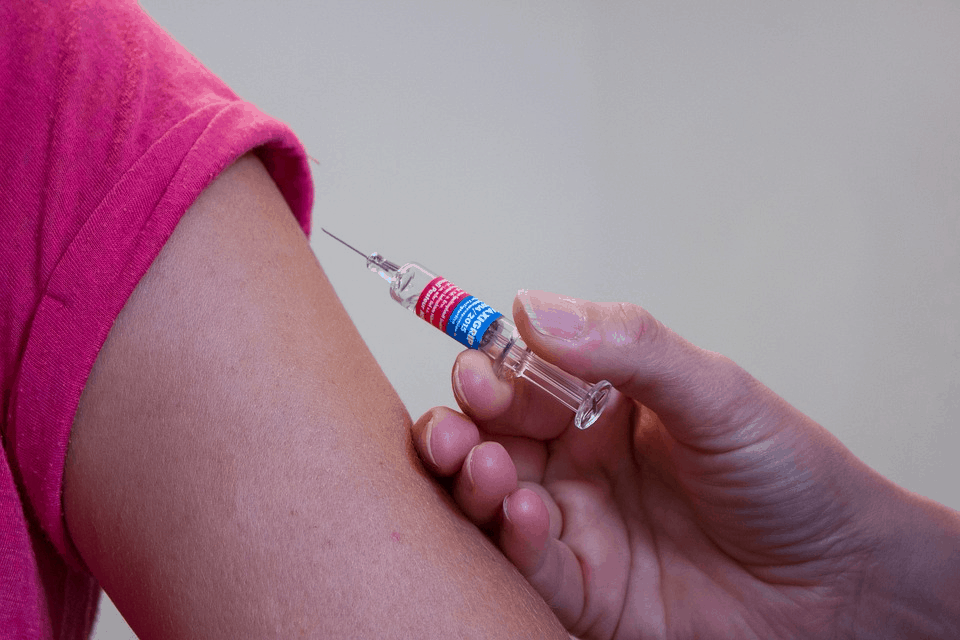
The Importance of Vaccines
Vaccines work by prompting the immune system to generate antibodies against any foreign invader without infecting you with a disease. Consecutively, when you encounter the same infection in the future, your body will be prepared to combat it.
Vaccinations educate your immune system by using a unique component of that particular pathogen; therefore, when the body is exposed to that pathogen in the future, you will have minimum to nil symptoms.
