Every year, millions of people are misdiagnosed, leading to delayed treatments, lost lives, and billions of dollars wasted. Some medical conditions are more frequently misdiagnosed than others. Knowing how to spot the signs of a bad diagnosis and when to advocate for yourself can help you avoid this all-too-common and potentially deadly error. These are some of the most commonly misdiagnosed health issues.
Heart Attacks and Strokes Are Misdiagnosed As Acid Reflux and Migraines
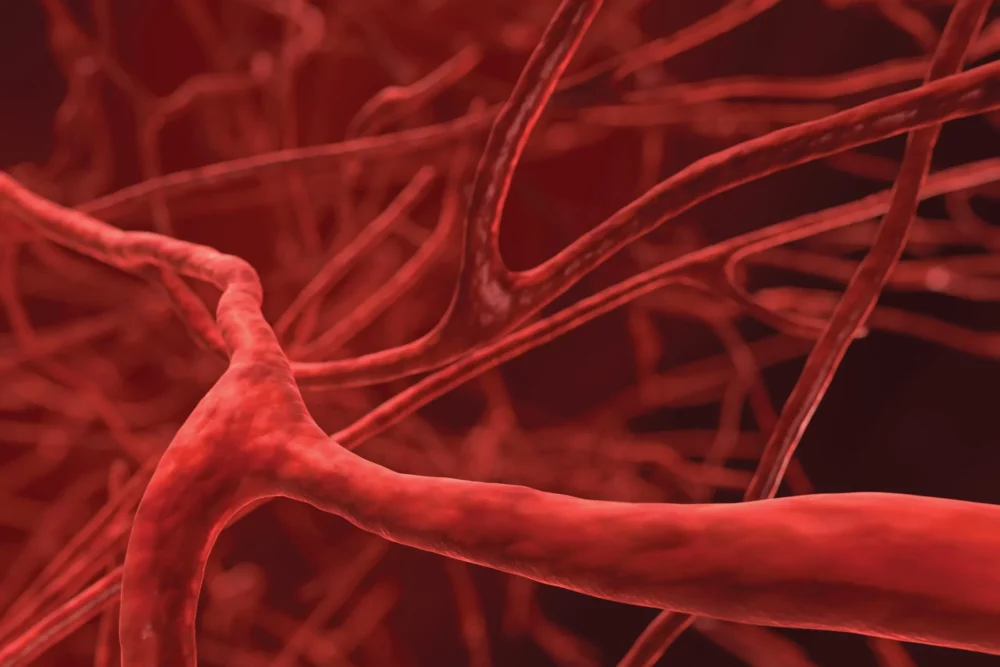
Blood vessels carry blood and oxygen to every part of the body. When they’re not functioning properly, it can spell serious trouble for your health. Diseases of the blood vessels, or vascular diseases, range from harmless conditions like varicose veins to life-threatening heart attacks and strokes. Because blood vessels affect every part of your body, vascular disease can have a wide variety of symptoms. This makes diagnosing vascular diseases particularly difficult, especially in emergencies. In fact, one study found vascular events like heart attacks and strokes are the most commonly misdiagnosed conditions in emergency rooms.
The most common cause of heart attacks is blockage of the blood vessels carrying blood to the heart. The chest pain and discomfort associated with heart attacks mimic much less serious conditions like acid reflux and angina, which occurs when heart muscles don’t get enough oxygen. Angina can also cause pain in the shoulder and abdomen, just as a heart attack can. Strokes are caused by blocked or burst blood vessels in the brain. Strokes can cause paralysis, numbness or weakness on one side of the body, dizziness, difficulty walking, severe headaches, and trouble seeing or speaking. Many conditions mimic these symptoms, including seizures, migraines, and functional neurological disorders, a broad category of brain disorders that result from disrupted communication between the brain and body.
